Blog

The last story I covered in-person without a mask was at Regional Council in early March 2020, as the government prepared to implement its pandemic response plan. I shook hands with someone on the way in, and sat maskless, one foot from then Acting Medical Officer of Health Dr. Hsiu-Li Wang for a candid conversation after the meeting. None of these things were out of the ordinary at the time.
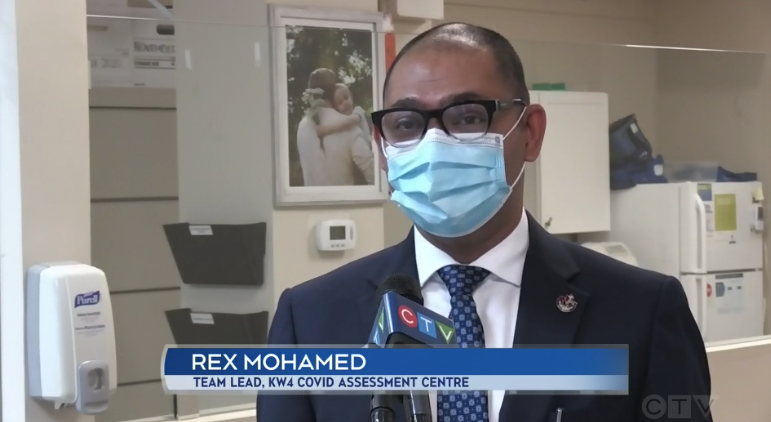
A delegate at the meeting caught my ears and eyes, as Rashid Mohamed (affectionately known as “Rex”) told council of his walk-in clinics’ woes and lack of personal protective equipment (PPE). Rex was not at the meeting to complain, though. Instead, he was there with an offer.
“One of our clinics is well-situated with ample parking spots,” said Mohamed in an interview at the time. “It could be a testing centre, it could be a screening centre, however they want to run it. To me, that would be an offer where I’m saying, ‘Let’s have a centre here, we take the load off the emergency room, and maybe we can also support it to run after hours. Eventually the goal would be to run it 24 hours if we can staff it.”
It was not long before the Region would take him up on that, in what would become a difficult but quick process.
“I won’t sugar-coat it and say that the process was an easy one,” Mohamed told 570 NEWS in a recent interview. “We had a lot of ground to cover in making sure that we had the right procedures in place for the centre, now known as KW4 COVID Assessment Centre.”
Swabbing stations had to be set up, staff completely re-trained, and PPE put in place to protect those staff. A shortage of PPE would also not be a problem for long for Mohamed.
“As soon as the word got out that we had a PPE crisis, and we were running out of PPE, the community outreach was so overwhelming,” said Mohamed. “We were touched by the amount of people who heard our story and reached out with messages of hope, as well as sending PPE as best as they could.”
He also credited Grand River Hospital and St. Mary’s General Hospital with their incredible support, both in training and in supplying PPE.
The KW4 assessment clinic also pioneered free transportation for those who needed to be tested, at first renting out a limo service. That plan had to be quickly adjusted as demand shot up. They ended up purchasing other vehicles, including former police cruisers.
That free transportation is now offered across the Region, and they have even provided some trips to Guelph.
It’s a good thing that Mohamed offered up his clinic, as demand reached an incredible level at the end of the summer, as the government announced that any COVID-19 symptoms in school children should result in the family getting tested.
“At one point I had to show up with a couple of our team members to try and request people to go away,” Mohamed recalled. “We had about 300 or so people lined up outside the clinic in the parking lot, in hope if they were not able to get an appointment.”
That clinic alone received some 3,600 calls through the COVID dispatch centre during that time.
Another busy spike was around two weeks after Christmas, where staff pulled double shifts to test twice as many patrons. Mohamed noted that the spike has died back down to the normal level of tests, about 200 per day.
“Every single day, some people say we’re crazy, why do we do this,” he said. “If we’re crazy, then the firefighter is also crazy. He runs into the fire when everyone is running out.”
Running into the heart of the crisis was something that Mohamed knew he had to do, with family who helped fight the SARS epidemic 17 years ago.
“We knew kind of what we were getting into, and we said, ‘We can do it, let’s do it now. And if we all come together, we’re going to be able to conquer this virus.’ And that’s what inspired us.”
Mohamed noted that he would be remiss if not to mention those who helped him and his team, with Dr. Heather Dixon and Dr. Joseph Lee being the “backbone” of the operation.
“I want to say a huge thank you to all the people who have helped us in making this project so successful. When I say that all hands were on deck to make this project a ‘go,’ that would be an understatement. The team support and guidance I’ve witnessed has been overwhelmingly amazing. I think that, together, we will be able to curb the spread of this virus. And, in doing so, help to keep our community safer. I think seeing as Martin Luther King Day just passed, it would be ideal to end off with a quote by him, in which he has most famously stated, ‘Life’s most urgent and persistent question is: what are you doing for others?’ And I can proudly say my team, my family, and I aided the wonderful and amazing healthcare leaders of this Region, and received the most precious opportunity to help and give back to the community which we are most grateful for.”
Link to story on CTV News – Jan. 22, 2021
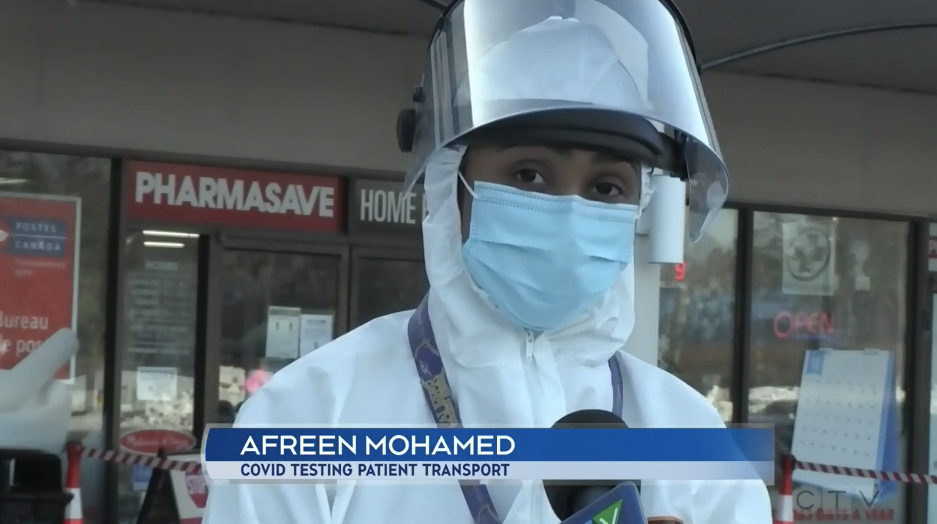
A free transport service to get a COVID-19 test has expanded across Waterloo region to now include Cambridge.
A driver picks up a patient from their home, drives them to a test site, and then back home again. The vehicle is sanitized between trips. The service is free for anyone who needs it and wants a test.
Link to story on CTV News – Jan. 18, 2021
KITCHENER — Community members continue to step up to help during the COVID-19 pandemic.
From a Cambridge doctor who helped her hospital prepare for the arrival of COVID-19 to a group of Waterloo researchers developing a needle-less vaccine, people are working hard to support one another this year.
CTV Kitchener is featuring work during the pandemic every Monday.
Read stories of people making sure we’re stronger together, even when six feet apart:
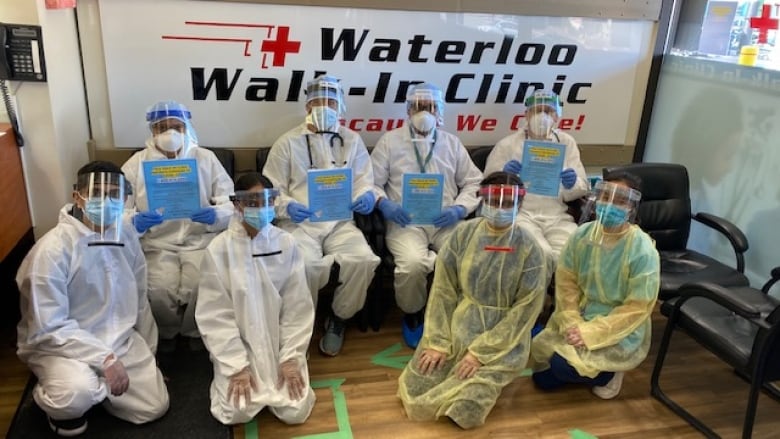
A Waterloo walk-in clinic transformed into a COVID-19 testing site in a week.
A local doctor is being praised for her work preparing Cambridge for the COVID-19 pandemic.
A teacher in Waterloo helped bring a classic board game to life.
A nurse who made sure her coworkers were taken care of during the first wave of the pandemic.
Link to story on CBC.ca by Joe Pavia – Jul 15,2020
“Patients called the clinic requesting masks after mandatory regional bylaw
The owners of three walk-in clinics in Waterloo and Kitchener are distributing 25,000 disposable masks to people who need them.
Rex Mohammed says he and his wife, Meera, took action after receiving a number of requests from people who needed a face covering.
The couple has purchased masks from a supplier, and will hand out them out at their locations at Westmount Place Walk-In clinic on Westmount Road, which is also a COVID-19 assessment centre; the Waterloo Walk-In Clinic on University Avenue; and the K-W Walk-In at the Boardwalk in Kitchener.
“When the [region’s mandatory mask] rules came in effect, we noticed a lot of patients and a lot of the random public would call in and request if we had any masks,” said Mohammed.
“They were having difficulty going for groceries and they did not have any masks. They wanted to come to the clinic but they didn’t have masks. They want to go get their prescriptions, they don’t have masks.So I said, ‘We’ve got to do something.'”
Mohammed says one disposable mask will be available daily for people who really need it.
‘You need to act to make a difference’
The walk-in location at Westmount Road was one of the first COVID-19 assessment centres that opened in the region for testing, Mohammed says. He said they’re now testing between 100 and 200 people a day.
Staff have also provided transportation to people who need a drive to get a test. About 180 people have taken them up on the offer, he said.
This isn’t Mohammed’s first time witnessing a pandemic. When he was a university student during the SARS outbreak in Toronto he watched members of his family in the medical field testing and attending to patients who were ill.
“One thing I’ve learned from that first experience is if you sit on it you will never be able to make a difference,” said Mohammed.
“If you act on it right away. You possibly will be able to tackle it down.” ”
· CBC News ·

Link to story in Waterloo Chronicle by Johanna Weidner – Jul 14, 2020
“Disposable mask available to anyone who can’t afford one now that they’re mandatory in Waterloo Region
WATERLOO REGION — Free face masks are being handed out by the owners of three local walk-in clinics, including a COVID-19 testing site.
They bought 25,000 disposable face masks that will be available starting Wednesday at the Waterloo Walk-In Clinic at 170 University Ave. W. in Waterloo and the K-W Walk-In Clinic at 100 The Boardwalk in Kitchener.
“Somebody had to do something,” said Rex Mohamed, who owns the clinics with his wife Meera Mohamed.
“You could feel the frustration,” Mohamed said. “Luckily we were able to source out a supplier.”
He is hoping their mask giveaway will encourage others to do the same as well to ensure everyone has access to a mask, in particular if they can’t afford to buy one.
“They’re very appreciative,” Mohamed said of those who have received a mask.
People are asked to only take one mask, due to the strain on personal protective equipment supplies during the pandemic. They’re available while supplies last during regular clinic hours from 9 a.m. to 8 p.m., but not at the testing clinic because that site sees patients by appointment only.
The couple have also been providing free transportation to the testing centre for anyone who needs it.
“Whatever we can do,” Mohamed said.”

Link to story on CTV News by Nicole Lampa – May 22, 2020
“KITCHENER — A COVID-19 assessment and testing centre in Waterloo is offering a free service to make it easier for residents with transportation issues to get tested.
An old ambulance has become a free ride for those like Lina Roult, who was tested at the KW4 Community Assessment Centre on Thursday.
“I’m so happy that this service exists because I don’t have a car,” she says.
In order to help prevent the spread of the virus on public transit, they initially rented a private limo service for patients who needed tests but had no way to get there.
Then he decided to purchase vehicles more appropriate to the task.
“These are ex-ambulances. We’ve bought two of those and we are transporting patients at no cost,” Mohamed explains.
Nearly 60 people have been transported to and from the clinic so far.
“My understanding is, it’s been received extremely positively,” says Dr. Joseph Lee.
Patients sit in the back of the ambulances and are provided masks.
The vehicles are sanitized between each patient, and drivers are required to wear personal protective equipment.
Mohamed’s wife had also stepped in as a driver up until Thursday.
“As a matter of fact, my wife is in the hospital right now. She was picked up by ambulance in the morning with chest pains and my daughter is showing some signs,” he says.
“But it’s not going to stop us. We’ll continue serving.”
For patients like Roult, the help is appreciated.
“It was a big relief because otherwise I’d have to have thought about walking up here, which is quite a long ways,” she says.
Last weekend, testing opened up to the general public—before then, it was prioritized for high-risk groups, like health-care workers or long-term care residents.
Certain locations are still by doctor referral only, while others, like ones at the hospitals in Kitchener, are working on self-referral options.”
Nicole Lampa CTV News Kitchener Videographer

Link to story by CTV News by Nicole Lampa – May 21, 2020
“WATERLOO — Those running the COVID-19 assessment and testing centre in Waterloo are offering a service that is making a big difference.
Mohamed teamed up with an area doctor to create the assessment centre, and originally rented a private limo service, but had no way to get there himself.
The K-W 4 Community Assessment Centre has since purchased vehicles to transport people to be tested.
The method is done in order to prevent the spread of the virus on public transit. Nearly 60 people have been transported to and from the clinic so far.
The vehicles are sanitized after each patient and drivers are required to wear PPE.
Mohammed’s wife had stepped in as a driver until Thursday.
“My wife is in the hospital right now,” he said. “She was picked up by an ambulance this morning with chest pains, and my daughter is showing some signs.”
“It’s not going to stop us. We’ll continue servicing whatever it takes.”
Linda Roult has tested for COVID-19 and says the ride is greatly appreciated.
“It was a big relief because otherwise I would have to walk here, which is quite a long ways,” she said. “Or I would have had not had a test, which is not good.”
The Waterloo assessment centre on Westmount Road is open for general population testing, but is still by referral only.”
Nicole Lampa CTV News Kitchener Videographer

The greatest passion of any medical professional is to cure their patients. The technological advancements at present have added a lot to the medical science and we have a variety of improved options for treatment, diagnosis, and prognosis of many diseases. Today, people consider doctors as their heroes and they believe that the present medical science can do any wonder. People entrust their doctors with their health conditions looking forward to them for possible solutions.
Nevertheless, we cannot deny death because every one of us is born to eventually die one day. Also, medical care facilities don’t bring positive results always. There are greater chances of side-effects of treatments leading to unfavorable conditions. This is sometimes when the doctors are questioned, especially when the patient is approaching the end of his life. In such conditions, some of the most difficult questions arise that need to be addressed for the patients but are ignored. These questions are mostly about the worth of the treatment for the patient, the expected quality of life, the benefits or harms of any particular treatment, etc.
All of these questions require the consent of the patient to continue with the treatment. Lack of the patient’s consent leads to the continuation of the suffering. The doctors cannot decide about these questions on their own because they had taken the oath of making every possible effort to save the life of their patients. This is why “discussions about the advance directives at the end of life care” are encouraged.
In addition, doctors have often witnessed a family conflict at the bedside of the patients. Half of the family insists to continue with the aggressive treatment while the others are of the opinion that the patient should be allowed to have a natural death without any harsh treatment. This happens usually when the patient is very old or too weak to respond to the treatment. These matters could be solved easily with the patient’s consent but he/she isn’t in a position to do so. This is only possible if the patient already discussed the advance directives at the end of his/her life care.
Discussions about the end of life care can bring numerous advantages for the patient, the family and the medical care staff associated with the patient. These discussions give an idea about the wishes of the sufferer regarding the end of life care. It removes a burden from the minds of the family members and they can choose the treatment as per the patient’s choice. Moreover, it helps the doctors to choose an appropriate treatment in time as well. It builds a sense of trust and comfort between the patient and those who are entrusted with his/her care. Most importantly, the discussions about the end of life care avoid unnecessary prolongation of suffering for patients with severe illnesses. It makes it a bit easier for them to die.
It is not always necessary to discuss the matter with the family. Of course, they are your loved ones and the thought of leaving them can grieve you all. You can discuss the matter with your family doctor. It is better to sign a legal document stating all your wishes and demands related to life care so that it can be shown to your family at the required time.
Most of the people consider the discussions regarding the end of life care important but only a few practice it. Considering COVID-19, it is the best time for such discussions. The spread rate of the virus is a threat that anyone can catch it. Anyone of us can end up sick with the Coronavirus. At present, it is such a traumatic disease that leaves the patient mentally crippled. They are not able to make decisions about their life care at such a critical point. It is very important for us to let our families know the level of the medical care we wish to have if we’re harmed with the virus. It is necessary to consider and communicate your wishes and beliefs earlier so that conflicts at your bedside are avoided.
Discussions about the end of life care can make a huge difference in the time of crisis. It is not about denying medical care regardless of age or condition. Also, it isn’t necessary that every one of us will encounter severe illnesses. It is just a healthy exercise that can help you to acquire the medical care of your own choice and avoid sufferings at the death bed.
Sources
The conversationproject.org (https://theconversationproject.org/tcp-blog/5-end-of-life-care-stats-everyone-should-know/)
Smeenk, F. W., Schrijver, L. A., van Bavel, H. C., & van de Laar, E. F. (2017). Talking about end-of-life care in a timely manner. Breathe, 13(4), e95-e102.
American Academy of Pediatrics, Committee on Pediatric Emergency Medicine, American College of Emergency Physicians, & Pediatric Emergency Medicine Committee. (2006). Patient-and family-centered care and the role of the emergency physician providing care to a child in the emergency department. Pediatrics, 118(5), 2242-2244.

Any pandemic or a disease outbreak is one of the greatest tests of any society. This hard time brings unusual inconveniences and adversities for the people living in the threatened area. Global pandemics lead to greater v2astation. They have long-term effects on almost all the sectors of life across the world. From declining the economy to stopping everyday life, a pandemic has a lot to do with the people. It creates political, economical, and social unrest all around the world.
One of the major effects of any pandemic is the deterioration of the public’s mental health. People experience a sense of fear, threat, anxiety, and restlessness all the time. Most importantly, self-isolation as a consequence of social distancing is reported to harm the mental health of the people. It is often associated with negative feelings and mental illnesses that in severe cases may cause the death of patients.
Man is a social animal. It cannot survive without social connections, communications, and interactions. There are very few people who live happily when isolated. However, the majority of the human population loves to interact. The power of even a momentary touch has long-lasting effects on human wellbeing. One cannot spend the whole life in a particular place with no one or a certain number of people around. It is a human psychological desire to go out in the world, meet new people and make connections. When you spend time with your family or when you go out with friends, you share your problems, everyday routines, your due tasks and what not? All of this interaction is scientifically proven to be cheering, therapeutic, and pain-relieving. However, we should never forget that every picture has two faces. Socializing is good if done with right and positive people. Interaction with negative-minded people is much worse than isolation!
Isolation and mental health
COVID-19 has made us all sit at homes and maintain a distance with the world. Unfortunately, this social distancing is one of the most effective preventive approaches towards pandemic. People who v2elop the disease or acquire the infection are also quarantined to limit the spread. The health care experts are continuously emphasizing on limiting human contact. People aren’t allowed to leave their houses until it is very necessary. All the markets have been closed down except for grocery stores, bakeries, hospitals, health care units, pharmacies, etc. People working at such places are also directed to maintain healthy distances for minimizing the chances of infection.
This state of isolation at homes is reportedly affecting the mental health of people especially the ones locked in their homes. The working members are disturbed due to their jobs and declining businesses. Children especially students are worried about their studies as they are unable to go to school, colleges or universities. Many of them must be missing their friends and the fun they had at schools or colleges. Everyone has mental health issues that they are battling in different ways. Doctors and paramedical staff working 24/7 in the hospitals are mentally exhausted. They are tired of living away from their loved ones and performing duties day and night. The patients of COVID-19 living at the quarantine centers are said to have the greatest mental health issues. The disease cuts their contact with the outer world which is not less than a trauma. They demand greater attention and empathy. The poor class of the society who used to work on daily wages is suffering the most. People don’t have anything to eat and no work which is very traumatic for them.
There are a lot of studies that indicate an increase in the rate of v2elopment of mental illnesses during isolation. Anxiety and depression are once again hitting people hard. The daily news regarding worldwide deaths creates a sense of mental unrest among the general population. This wave of fretfulness mixed angst is decreasing the morale of people and compels them to surrender before the disease. The disease might not catch them but their fear of catching it makes the situation more miserable. People who have already fallen prey to numerous mental illnesses depict much worse symptoms! All of these responses are much obvious and expected but, if not controlled in time, they can lead to unexpectedly dangerous outcomes.
What needs to be done?
It is necessary to treat the disease but it is more important to motivate the people to fight it. COVID-19 might not be curable but at least we can fight it with motivation. The health care staff should ensure some safety measures concerning the mental health of the population. The perceptions of the patient about the situation can help them to fight both isolation and the disease very well.
Here we present a few tips to fight mental illnesses during the isolation.
One of the key tips to avoid mental illnesses is to prevent them from v2eloping. Don’t let yourself to consume your mind over negative imagination. Keep your thoughts positive and hopes high. Practice isolation creatively! Invest your time in creative work. Make friends with yourself and your family members and spend quality time with them. Try to spend your day doing what you always wanted to or what you love to do. Parents should motivate their children to practice healthy hobbies. Children should help their parents with household chores. Eat healthy food. Keeping all the tensions aside, try to take out some time to meditate. Make a regular exercise schedule, encourage your children to work out with you too. The infected people, living in quarantine, should not panic and fight the disease with strength. The medical staff shouldn’t only treat them but also empathize with them. If possible, they should let the patients contact their family members over phone calls.
We all need to understand that we are together in this hard time. We should support each other with all the available resources and pray for the health of the whole world!
Sources
- CDC, Coronavirus, 2019 (https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html)
- HUB, John Hopkins University, 2020 (https://hub.jhu.edu/2020/04/06/dani-fallin-mental-health-challenges-coronavirus/)
- WHO, Coronavirus-mental health consideration, 2020 (https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf)
- Global news (https://globalnews.ca/news/6776142/covid-19-pandemic-mental-health/)
- Venkatesh, A., & Edirappuli, S. (2020). Social distancing in covid-19: what are the mental health implications?. Bmj, 369.
Every pandemic comes with different life-long lessons for the whole world! It is the time of hardship and adversity, where the entire globe suffers from a greater crisis. Every outbreak challenges the world in a different way, confronting the experts with cerebral tests and trials.
Today, all the people across the world are threatened with COVID-19! The tiny monster named Coronavirus has locked down the whole world. It is spreading among people unstoppably and its daily growth chart has already reached the peaks! At present, it is the hottest topic of study and talks around the world. The worldwide scientific community is putting a continuous effort in controlling the spread and trying to figure out a suitable vaccine or cure, however; it couldn’t succeed yet!
COVID 19 is not the first pandemic to be reported. The world has already seen some of the deadliest pandemics in the past. For instance, the bubonic plague in the mid-1300s, the Spanish flu during 1918, the Ebola outbreak in 1976, the SARS pandemic in 2003, the Swine flu in 2009, the MERS syndrome in 2012 are some popular outbreaks of the past. All of these outbreaks had huge effects on the global health and economy and left an unforgettable image on the history of the world as well.
In this respective article, we present a thorough comparison among COVID 19 and these past pandemics or outbreaks including SARS, MERS, Spanish flu, Swine flu, Ebola, etc. One interesting thing to note is that all of these outbreaks except bubonic plague were caused by viruses and most of them reported respiratory disorders in the infected individuals. The initial symptoms reported are also very similar including fever, chills, cough, flu, etc.
The bubonic plague is famous as “BLACK DEATH”. It is considered one of the most v2astating outbreaks which resulted in the death of 75 to 200 million people in Eurasia and North Africa. Second to it is the 1918-Spanish flu which infected almost one-third of the world’s population with a death rate of 3-5%. Later, the world faced the outbreaks of viruses like SARS, MERS, H1N1-swine flu, Ebola and now the novel coronavirus!
In comparison with the past outbreaks, the rate of causalities due to COVID-19 is relatively low. Black Death is the biggest pandemic known to humans to date because it caused the death of almost 30-50 percent of infected people. The drastic effects of such a pandemic lasted for a long long time. However, COVID-19 is nothing like that. According to John Hopkins University, 381,000 cases of COVID-19 have been confirmed and16000 deaths have been reported yet. Countries like China, Italy, the USA, and Spain have been reported with the greatest death rate.
Apart from the death rate, there are many other factors comparable among these pandemics.
COVID-19 is somewhat similar to the past outbreaks with respect to its origin, the behavioral comeback of the society, and its possible outcomes on the global economy. Like other infectious diseases, it has a zoonotic origin of transmission however, its rate of transmission is much greater than the previous pandemics. This is probably because of globalization and rapid transportation across the world.
The social responses subsequent to the present pandemic are very much similar to the past outbreaks. The common human responses towards the disease include denial of the present condition, sense of anxiety, panic, and flight, racism towards the infected people, passing on rumors about the disease, racial intolerance towards foreigners especially Chinese, etc. Some people are taking advantage of the condition and using it as an opportunity for their business. For instance, the protection of masks and sanitizers are being sold at triple prices! On the other hand, there are some people tensed due to businesses closing all over the world. A part of the society is also working to help others e.g. the social welfare societies are setting up camps for the needy ones. A part of the upper class is voluntarily helping the lower class with the basic necessities of life.
One of the most common things about all of these pandemics is the preventive approach towards them. Social distancing has been observed as the best approach to prevent the present infection and the ones reported in the past. Every time, the world faced a pandemic, people are asked to stay home until the condition is controlled. Every pandemic demanded the people to travel less, consume less, and slow down their lives.
This social distancing also led to the global shutdown which had obvious impacts on the economy worldwide. According to the experts, the global economy is always expected to shrink in such unusual times. Almost all the sectors of livelihood are affected. The v2eloping states and countries are always at greater risks due to the declining rate of employment and decreased incomes.
The fallout of every pandemic is always dependent on factors like the time at which it is identified, the extent to which it is fatal or contagious, the lifestyle of the population exposed to the diseases, and most importantly how quickly people find an available cure for it.
Pandemics are not less than wars. In such difficult times, the medical staff of any place works as an army to protect their people and their lives. The same is the case with COVID-19, it has put the medical staff across the world at a great test and they are putting all their effort to combat the disease as well. One such example is the waterloo walk-in clinic. They have developed a COVID-19 assessment center for the people infected with the coronavirus. The Westmount place walk-in clinic has been turned to the assessment center. People can access it through a referral obtained by a physician, walk-in clinic, etc.
Sources
- WHO (https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—3-march-2020)
- CDC (https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html)
- Arizona daily wild cat (https://www.wildcat.arizona.edu/article/2020/03/n-covid-comparison)