Blog

Link to story on CTV News by Jennifer K. Baker – Apr 6, 2020
“KITCHENER — The Region of Waterloo announced Monday that it is opening two new COVID-19 assessment clinics.
One has been set up at the Westmount Walk-In Clinic, at 50 Westmount Road North in Waterloo.
Public Health says the site will serve the communities of Kitchener, Waterloo, Wellesley, Wilmot and Woolwich.
The second location is at Cambridge Memorial Hospital at 700 Coronation Boulevard, and will accept patients from Cambridge and North Dumfries.
However Public Health is warning that these sites are not testing centres and walk-ins are not welcome.
Dr. Hsiu-Li Wang, the acting Medical Officer of Health for the region, says people should only go the assessment centres if they get the go-ahead from their family doctor or healthcare provider.
She says residents should first visit the province’s online self-assessment tool to determine whether they should seek a clinical assessment.
They can then set up a phone or online appointment with their family doctor or walk-in clinic healthcare provider.
If that doctor determines that an in-person assessment is required, they will refer the patient to one of the region’s new assessment centres.
Dr. Wang says this system has been set up for those with moderate symptoms and anyone with severe symptoms should go to their local hospital.”
Jennifer K. Baker CTV News Kitchener Writer-Reporter

Link to story on Kitchener Today by Ben Eppel – Mar 12, 2020
“The goal is to open community assessment centres as the Region implements its Pandemic Response Plan
COVID-19 was finally declared a pandemic on Wednesday as cases of the new coronavirus continue to increase globally.
That means Waterloo Region is implementing their Pandemic Response Plan from 2008, something councillors describe as similar to the Regional Emergency Response Plan.
The most significant part of that plan involves “community assessment centres,” the need of which is greater than first appears.
The only place we can assess people for COVID-19 is in our hospitals at the moment, according to Dr. Hsui-Li Wang: Acting Medical Officer of Health for Region of Waterloo Public Health and Emergency Services.
“When this virus started to make an appearance, the Ontario Ministry of Health decided to put in very high levels of precautions, in order to protect health care workers and other patients. Because of that, really, currently, the only place that’s able to assess and test clients under such stringent conditions are hospital environments,” explained Wang in an interview. “The government recognizes, with the increasing number of cases, that’s not a sustainable solution. We’re currently in discussions with them to allow us to help move some of the testing into a community location. They are supportive of that.”
People currently need an appointment to get screened at a hospital according to Cheryl Evans, manager of Communications and Engagement for Grand River Hospital.
“This is not a walk in clinic,” said Evans in a statement. “We have worked with Public Health to develop a temporary solution to isolate screening and testing for COVID-19 to one area of the hospital as much as possible. Patients should first be screened and determined to need an appointment for testing by the emergency department, by public health, or through their family physician in consultation with public health. We are working with our health system partners, public health and St Mary’s General Hospital to plan for a community clinic. No timeline for this yet but we should know more by Friday.
Wang said it made sense in the earlier days of the virus to take high precautions and screen in hospital, but now that the virus is more understood, it’s an unnecessary strain on the hospital.
“We have a better understanding of how it spreads,” said Wang. “We think, going forward, it makes a lot of sense to be able to assess and test these people in a community setting. We’re working right now with the hospitals and our primary care partners to try to identify locations in the community where we can assess people. These are the people who come back from travel, they’re the most at risk, and develop symptoms, but aren’t well enough to be assessed in the hospital environment.”
As if by fate, one of those locations presented itself at the meeting.
Rashid Mohamed, also known as “Rex,” is the owner and operator of Waterloo Walk-in Clinic, Westmount Medical Centre and KW Walk-in Clinic.
He offered to completely shut down one of his clinics to walk-in services to convert the space to community assessment.
“One of our clinics is well-situated with ample parking spots,” said Mohamed in an interview. “It could be a testing centre, it could be a screening centre, however they want to run it. To me, that would be an offer where I’m saying, ‘Let’s have a centre here, we take the load off the emergency room, and maybe we can also support it to run after hours. Eventually the goal would be to run it 24 hours if we can staff it.”
Dr. Wang might just take Mohamed up on his offer.
“Absolutely, we’re open to any and all ideas,” said Wang. “We have had family physicians start to step up and offer ideas and we’re very willing to hear from them, and to work with them. Those clinics will need physician resources, nursing resources, and if we can have our primary care physicians in the community pitch in and help us find a solution, that would be great.”
The council meeting wasn’t an entire picture of optimism, however.
Mohamed originally was a delegate at the meeting to tell council how strapped his clinics are for equipments such as facemasks.
Doctor Terry Polevoy also took to the podium, painting a similar grim picture.
In an interview, Mohamed told of his frustrating phone conversations with suppliers, saying that he was first told to “wait until you’re within 10 days of losing supplies,” then seven days, and finally being told that masks are for high priority areas only.
This all came despite his clinic burning through twice as many masks as usual.
“I don’t know how they’re describing ‘high priority areas’ versus low priority. We’re three cities here. We see patients from anywhere and everywhere. Somebody who’s sitting behind a desk is giving me the logic, telling me to ‘direct the patients to make a phone call. Direct the patients to public health.’ How do I do that? Do I stand outside my door? At all three clinics with the patients outside? This is a walk-in clinic. The patients who are sick, they don’t look up on Google, they don’t look up the news channel, they go to a doctor’s office [the clinic]. People don’t even stop at the pharmacy, they want to come here to hear it from the horse’s mouth.”
Dr. Wang said the Ministry of Health is working on the equipment shortage.
If the Region does take Mohamed up on his offer, it would take a bit of time to verify that all the resources are in place.
“It’s probably not going to take weeks, more a matter of several days to start up these community assessments,” said Dr. Wang. “We have to submit proposals to Ontario Health, and they obviously are going to take a look at this as quickly as they can.”
One of the main messages that public health is trying to get out to the public: call first. That will help you to stay informed and get early instructions, and reduce the strain on our healthcare system.
You can also find helpful, easy-to-read resources on the Public Health Website.
Waterloo Region’s 24-Hour Phone Line, and Public Health: 519-575-4400.”
By: Ben Eppel

Link to story on Waterloo Chronicle by Samantha Beattie – Dec 14, 2016
“A new walk-in clinic in Waterloo will help students, seniors and everyone in between avoid the emergency room.
“We’re just so excited about what’s happening here today, it’s something every community dreams about, having more medical facilities and better medical facilities,” said Waterloo Mayor Dave Jaworsky at the clinic’s opening last Friday.
Westmount Place Walk-In Clinic, at 50 Westmount Rd., has good timing. It was ready for business a week and a half after the auditor general’s report was released, which described emergency rooms as overcrowded and wait times as too long. Grand River Hospital also recently announced it would be taking the “rare” step of asking for donations in order to hire another emergency room resident.
“We know we are in a crisis from an emergency room perspective if our hospital is fundraising for an emergency room resident,” said Waterloo NDP MPP Catherine Fife at the opening.
“Having urgent care centres like this, which are community based, is an important asset we need to have in more communities across the province.”
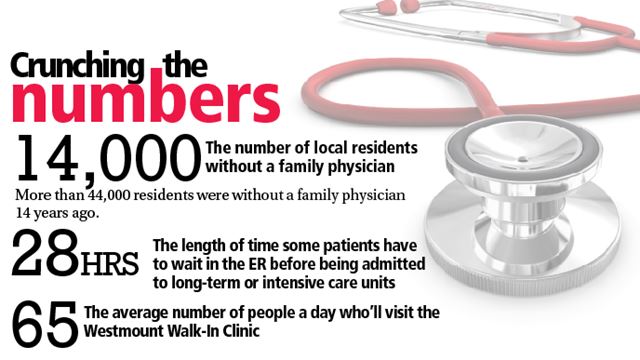
Waterloo Region and Woolwich Township have about 14,000 residents without family physicians, said Ian McLean, president of the Greater Kitchener-Waterloo Chamber of Commerce. While that may seem like a lot, 14 years ago more than 44,000 residents were without family physicians.
“The shortage of doctors was becoming a problem for business leaders looking to recruit and retain talent in the tech sector and also across other industries like accounting, law, banking and insurance,” said McLean. “People weren’t interested in coming to Waterloo if they couldn’t get primary care.”
A family physician is the entry point into the health care system. If there’s a shortage of those, more people have to resort to the emergency room to treat illnesses and get prescriptions or referrals to specialists.
“More and more physicians are nearing retirement age,” said McLean. “We have to recruit seven or eight doctors ever year just to tread water.”
And the competition is stiff.
“What we know is when doctors graduate they can go wherever they like. They’re in demand across the region, the province, the country and frankly North America,” McLean said. “We’re competing against everybody.”
Walk-in clinics are a kind of a stopgap measure.
“In the tri-city there are deficiencies in family doctor practices,” said Rex Mohamed, founder of the new clinic. “Walk-ins bridge that gap and take a load off of emergency rooms.”
From running several other walk-in clinics in the Waterloo region, he expects 50 to 80 people will visit the Westmount clinic every day. That’s 50 to 80 people who’ll avoid the emergency room and free up much-needed space.
Auditor general Bonnie Lysyk reported at the three hospitals she visited, patients were placed on “uncomfortable stretchers or gurneys in hallways and other high-traffic areas that were never designed for patient care.”
Nine out of every 10 patients in the emergency room went home after being treated. The majority were released between three and six and a half hours.
But for the one out of every 10 patients who needed to be admitted to the long-term or intensive care units for further treatment, wait times in the emergency room (or in hallways) could be as long as 28 hours.
Dr. Terry Polevoy and Dr. Richard Irvine are among the physicians who’ll be working at the Westmount clinic. Both have long careers in medicine and have watched the healthcare system change.
“It’s almost impossible for new people to Waterloo Region to find new physicians,” Polevoy said. “Luckily for them, they’ll find services here.” ”
Samantha Beattie is a reporter with the Toronto Star.